How to make a safeguarding referral
This section contains guidance and information about differentiating between poor care and potential safeguarding issues, and what to do and how to make a referral if something is a safeguarding concern.
Differentiating between poor care and potential safeguarding issues
Defining abuse can be complex, but it can involve intentional, reckless, deliberate or dishonest acts by the perpetrator.
Abuse or neglect can take place in any type of setting, but safeguarding is not a substitute for:
- providers’ responsibilities to provide safe and high-quality care and support
- commissioners regularly assuring themselves of the safety and effectiveness of commissioned services
- the Care Quality Commission ensuring that regulated providers comply with the fundamental standards of care or by taking enforcement action
- the core duties of the police to prevent and detect crime
There are incidents of poor care, or concerns about regulatory issues, that are separate from the safeguarding concerns reported to the Local Authority, and which need to be addressed appropriately.
The nature and timing of the intervention and who is best placed to lead will partly be determined by the circumstances. For example, where there is poor, neglectful care or practice by an individual member of staff, then an employer-led disciplinary response may be more appropriate. Commissioning or regulatory enforcement action may also be appropriate.
Below are some examples demonstrating the difference between poor care and abuse or neglect. Poor care might include:
- a one-off medication error (although this could, of course, have had very serious consequences)
- an isolated incident of under-staffing, resulting in a person’s incontinence pad not being changed in a timely manner
- poor quality, unappetising food
- one missed visit by a care worker from a home care agency (although this could, of course, have had very serious consequences)
Consider:
- Could this matter be addressed by the provider?
- Could this matter be addressed by the commissioner through a contractual or quality management approach?
- Is this a regulatory issue that needs to be reported to the Care Quality Commission?
There should be careful analysis to understand what is intentional and what is unintentional harm. However, where there is unintentional harm due to a lack of guidance for staff, this may also constitute organisational abuse.
Staff employed by NHS organisations or Somerset Council should notify the Councils Quality Assurance team of any quality concerns about an adult social care service via the Service Quality Feedback form.
Remember:
Potential indicators of a safeguarding concern that you need to act on might include:
- a series or pattern of medication errors
- an increase in the number of visits to Accident and Emergency, especially if the same injuries happen more than once
- changes in the behaviour and demeanour of adults with care and support needs
- repeated failure to support someone with eating and drinking
- clothes and person being dirty/unkempt
- repeated missed visits by a home care agency
- an increase in the number of complaints received about the service
- an increase in the use of agency or bank staff
- a pattern of missed GP or dental appointments
- an unusually high or unusually low number of safeguarding alerts
(this list is not exhaustive and could apply to one person, within an individual service or across multiple services operated by the same provider)
Recognising safeguarding concerns
All staff and volunteers working with adults at risk of abuse must know how to recognise abuse or neglect, and know who in their organisation they must report concerns to.
Safeguarding adults is everybody’s responsibility. If you recognise abuse or neglect, you must discuss it with your manager or your organisation’s safeguarding lead immediately.
In an emergency situation do not delay. If you are unable to contact your safeguarding lead, ring 999 for assistance.
What to do if you recognise abuse or neglect:
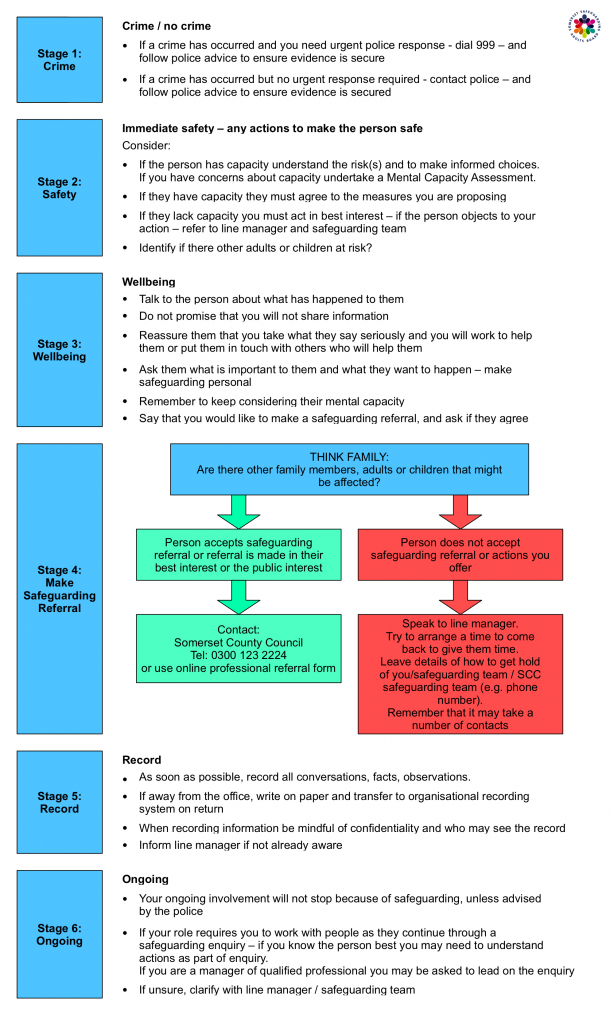
Stage 1: Crime
- If a crime has occurred and you need urgent police response, please dial 999 and follow police advice to ensure evidence is secure.
- If a crime has occurred but no urgent response is required, please contact the police and follow their advice to ensure evidence is secured.
Stage 2: Safety
Immediate safety – any actions to make the person safe
Consider:
- If the person has capacity to understand the risks and to make informed choices.
- If you have concerns about capacity, they must agree to the measures you are proposing.
- If they lack capacity you must act in their best interest. If the person objects to your action, please refer to the Line Manager and Safeguarding Team.
- Identify if there are other adults or children at risk.
Stage 3: Wellbeing
- Talk to the person about what has happened to them.
- Do not promise that you will not share information.
- Reassure them that you take what they say seriously, and you will work to help them or put them in touch with others who will help them.
- Ask them what is important to them and what they want to happen. Make safeguarding personal.
- Remember to keep considering their mental capacity.
- Say that you would like to make a Safeguarding Referral and ask if they agree.
Stage 4: Make Safeguarding Referral
Think Family: Are there other family members, adults or children that might be affected?
If yes:
- Person accepts safeguarding referral or referral is made in their best interest or the public interest.
- Contact Somerset Council. Phone 0300 1232224 or use online professional referral form.
If not:
- Person does not accept safeguarding referral or actions you offer
- Speak to your Line Manager. Try to arrange a time to come back to give them time.
- Leave details of how to get hold of you, Safeguarding Team or Somerset Council Safeguarding Team (for example, phone number)
Stage 4: Record
- As soon as possible, record all conversations, facts, observations.
- If away from the office, write on paper and transfer to organisational recording system on return.
- When recording information, be mindful of confidentiality and wo may hear the recording.
- Inform line manager if not already aware.
Stage 6: Ongoing
Your ongoing involvement will not stop because of safeguarding, unless advised by the police.
If your role requires you to work with people as they continue trough a safeguarding enquiry. If you know the person best, you may need to understand actions as part of the enquiry.
If you are a manager or a qualified professional, you may be asked to lead on the enquiry.
If unsure, clarify with your Line Manager or Safeguarding Team.
How to make a safeguarding referral
- Telephone 0300 123 2224 (Monday to Friday 8am to 6pm, Saturday and Sunday closed)
- Email adults@somerset.gov.uk
- or complete the Professionals safeguarding referral form
The phone number for Adults and Mental Health out of hours is 01823 368 244
Referrers should be notified of the outcome of the referral in a timely manner.
At all points during a referral, and if applicable a subsequent enquiry, staff must ensure that they consider the views of the individual by Making Safeguarding Personal and document how they have done this, particularly where a decision is taken to override them.
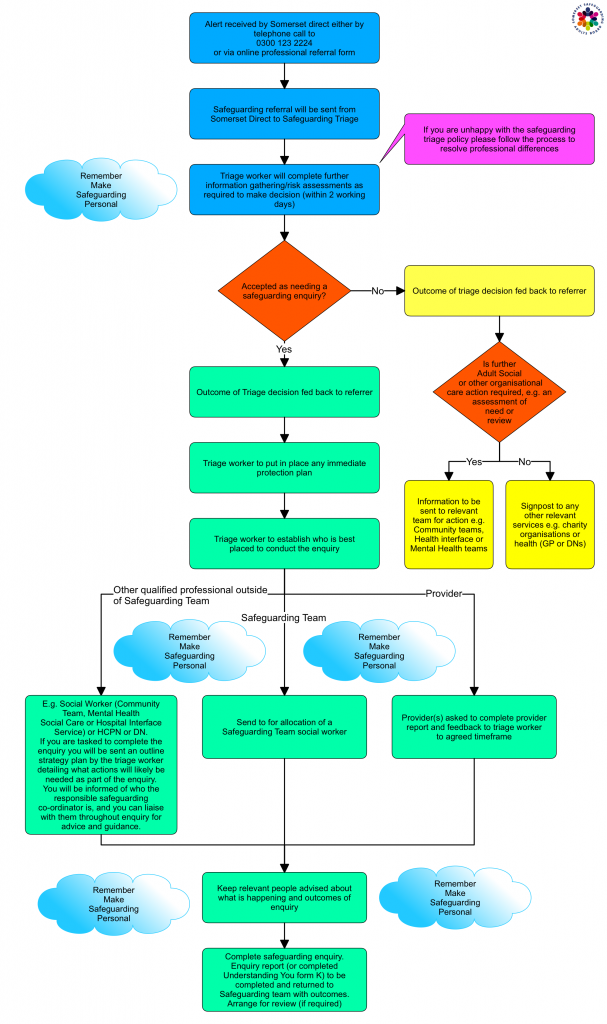
Step one:
Alert received by Somerset Direct, either by phone call to 0300 123 2224 or using online professional referral form.
Step two:
Safeguarding referral will be sent from Somerset Direct to Safeguarding Triage
Step three:
Triage worker will complete further information gathering risk assessments as required to make a decision (within two working days).
- If you are unhappy with the safeguarding triage policy, please follow the process to resolve professional differences.
Step four:
Accepted as needing a safeguarding enquiry:
If yes:
- Outcome of Triage decision is fed back to the referrer
- Triage worker to put in place any immediate protection plan
- Triage worker to establish who is best placed to conduct the enquiry
Other qualified professional outside of Safeguarding Team:
For example, Social Worker (Community Team, Mental Health, Social Care or Hospital Interface Service), Health Care Providers Network or DN.
If you are tasked to complete the enquiry, you will be sent an outline strategy plan by the triage worker detailing what actions will likely to be needed as part of the enquiry. You will be informed of who the responsible safeguarding coordinator is, and you can liaise with them through enquiry for advice and guidance.
Providers are asked to complete provider report and feedback to triage worker to agreed timeframe.
Step five:
Send for allocation of a Safeguarding Team social worker.
Step six:
Keep relevant people advised about what is happening and outcomes of enquiry.
Step seven:
Complete safeguarding enquiry. Enquiry report (or completed Understanding You form) to be completed and returned to Safeguarding Team with outcomes. Arrange for a review (if required).
Remember: Make Safeguarding personal
If not:
- Outcome of triage decision is fed back to the referrer.
- Is further Adult Social or other organisations care action required (for example, an assessment of need or review)?
-
- Yes: Information to be sent to the relevant team for action (for example, Community teams, Health interface or Mental Health teams)
- No: Signpost to any other relevant services (for example, charity organisations or health organisations such as GP or DNs)
Sharing Information and Consent
Empowerment involves a proactive approach to seeking consent, maximising the person’s involvement in decisions about who information is shared with, their care, safety and protection and this includes decisions regarding raising a Safeguarding concern.
Safeguarding Practitioners who co-ordinate the safeguarding adult process will ensure the adult at risk is involved appropriately, and that consent to actions required under the safeguarding process are discussed and negotiated with the individual as needed.
These can be complex decisions. If you are in any doubt you must either:
- Seek the advice/ support of your line manager/supervisor or organisational safeguarding lead
- Contact the Local Authority’s Adult Safeguarding Service
- For staff who are in regulated professions, their own regulators and professional body will also offer advice and guidance in these instances
See also:
- General Medical Council
- Health and Care Professions Council (HCPC)
- Nursing and Midwifery Council
- Care Quality Commission
It is always essential in safeguarding to consider if the adult at risk is capable of giving informed consent. If they are, their consent should be sought. This may be in relation to whether they give consent to:
- A safeguarding concern being raised. Where an adult at risk with capacity has made a decision that they do not want a concern to be raised and there are no public interest, legal restriction or duty of care considerations and nobody else is at risk, their wishes should be respected. The person must be given information, have the opportunity to consider the implications of their decision and understand the likely consequences of their decision over the short and long term
- A Safeguarding Adults enquiry going ahead in response to a concern that has been raised. Where an adult at risk with capacity has made a decision that they do not want action to be taken and there are no public interest or vital interest considerations, their wishes must be respected. The person must be given information, have the opportunity to consider the risks and understand the likely consequences of their decision over the short and long term
- An individual safeguarding plan being put in place
- A medical examination
- An interview
- Certain decisions and actions taken during the Safeguarding Adults process with the person or with people who know about their abuse and its impact on the adult at risk.
This is not an exhaustive list
In addition, it is essential to consider the consent of the adult at risk to an activity that may be abusive – if consent to abuse or neglect was given under duress, for example, as a result of exploitation, pressure, fear or intimidation, this apparent consent should be disregarded.
If, after discussion with the adult at risk who has capacity, they refuse any intervention, their wishes will be respected unless:
- There is a public interest, for example, not acting will put other adults or children at risk
- There is a duty of care, public or vital interest, for example, a serious crime has been or may be committed
Recording concerns and preserving evidence
Ensure that all written records are dated, signed and stored confidentially and securely.
Written records should state the facts – what you have seen and heard. Opinions and assumptions must be avoided. The individual’s own comments should be written in their own words and not paraphrased or interpreted by the person recording the conversation. If the individual has stated what support they feel they need to be safe, or what outcomes they wish to achieve, these must also be recorded.
In cases of physical or sexual assault, try to persuade the individual not to wash, bathe or shower until the Police or doctor has seen them. Do not attempt to tidy or clean the immediate environment – leave things as you find them and await instructions from the investigation team. Gather as much information as you can. Do not delay in making a referral, even if you do not have all of the information available.
Information gathering
This stage should not be commenced if a criminal offence has occurred and is under investigation by the police without consultation with the police officer in charge of the investigation to discuss procedures and actions, what to do and when. The more serious the actual or possible offence, the greater the need to notify the police as soon as it is discovered.
What to do if it isn’t safeguarding
It is important to discuss your concerns if you are not sure of next steps.
To do nothing is never an option.
More Information and Guidance
- Making decisions on the duty to carry out Safeguarding Adults enquiries – Local Government Association
- Resources to support Making Safeguarding Personal – Local Government Association
- Is my resident well? Ten everyday questions to help care home staff and carers, recognise signs of residents becoming unwell – NHS


